Shoulder Instability
Overview
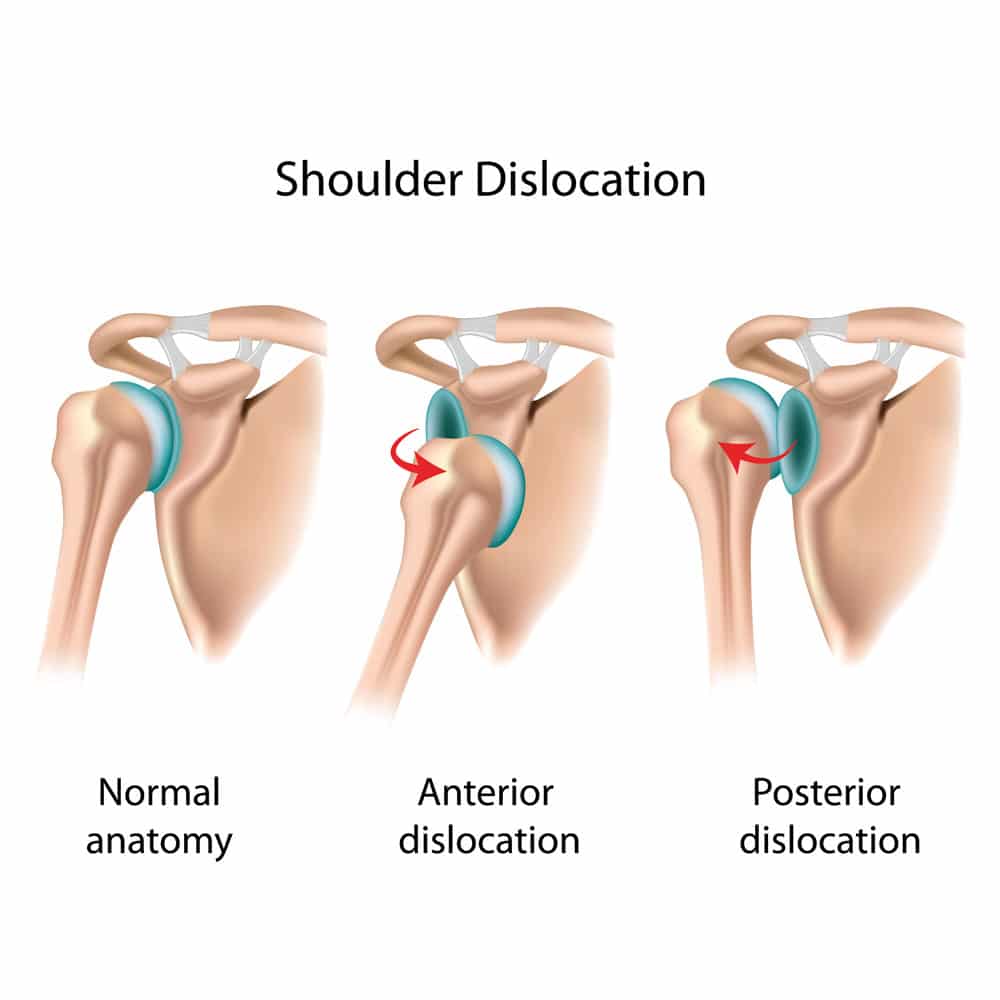
The shoulder is a very mobile joint. The main ball and socket joint is called the glenohumeral joint (GHJ) and this is the one that is most commonly dislocated in trauma and sporting injuries. This is because the socket is very shallow. The socket is augmented with a soft tissue bumper called the labrum. Ligaments and the capsule are attached to and around this. When a dislocation occurs, these structures are injured and may need repair.
Treatment
Most frequently the injury is in the front of the shoulder and is called a Bankart lesion. Usually this is amenable to a soft tissue repair which in my hands is usually done with a keyhole ‘arthroscopic’ technique.
Sometimes the pathology involves bone loss or stretched ligaments which can mean open surgery or bone transfer surgery is more suitable to minimise the risk of recurrent instability after surgery. Nonetheless all procedures for instability are risk reduction procedures rather than risk elimination procedures.
For example, in young contact athletes, we can aim to reduce the risk of further instability events from over 90% to less than 10% but cannot offer no risk. Every shoulder is slightly different. After clinical examination and review of your imaging I will be able to discuss the option that I think will best suit your pattern of instability with you.

Aftercare
The muscular elements of the shoulder such as the rotator cuff are very important to stability and good rehab is key to maximising your stability and function post operatively. It is important that you engage with your physio in the post-operative phase. Most of the time, gentle motion is allowed but there will be a period during which you will need to wear a sling and limit your activities to protect the surgical repair.
Return to play for athletes, particularly contact athletes varies with the procedure involved, the sport involved and the progression through rehabilitation. In general, a return to play in the order of 4 and a half months or sometimes a little less is usual, however.
Patients: see our advice sheets on what to expect from your procedure and how best to manage afterwards
Physios: see our therapy guidelines for post-operative care

